Health
FDA Changes COVID Vaccine Policies, Limits Access for Under-65s
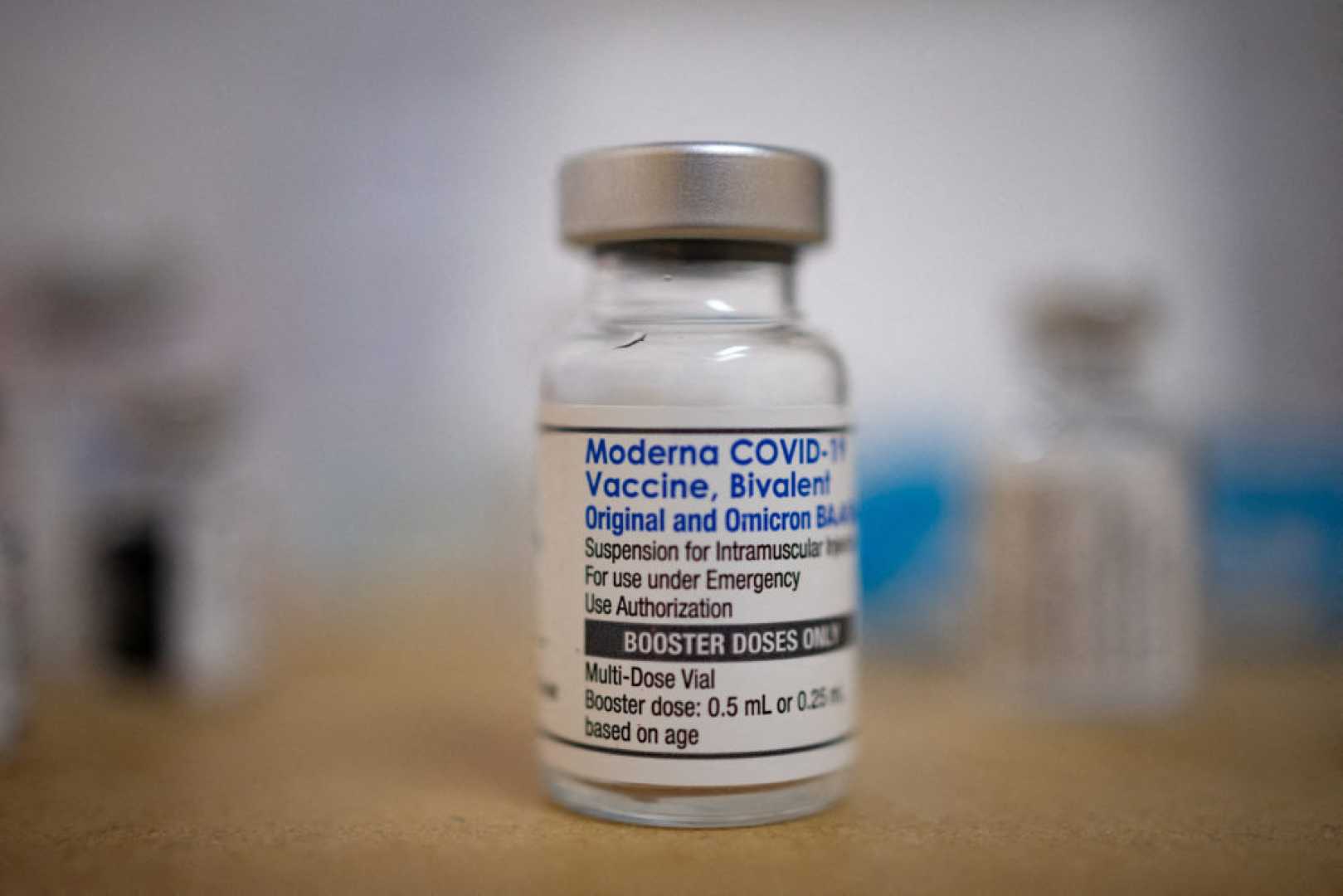
WASHINGTON, D.C. — The Food and Drug Administration (FDA) announced Tuesday a significant shift in its approach to COVID-19 vaccines, restricting access for healthy Americans under 65 years old. The new policy aims to prioritize older adults and those with medical conditions that elevate their risk of severe illness from COVID-19.
Under the revised guidelines, vaccines will still be available for adults aged 65 and older, as well as for individuals over six months with certain health issues. However, the FDA will require vaccine manufacturers to conduct additional clinical trials before approving shots for younger, healthy adults, as stated in an article published in The New England Journal of Medicine.
“We have launched down this multiyear campaign of booster after booster … without gold-standard science to support this for average-risk, low-risk Americans,” said Dr. Vinay Prasad, director of the FDA’s Center for Biologics Evaluation and Research. The intent is to restore public trust in vaccines and align U.S. policies with other high-income countries, which have long adopted a risk-based approach.
The new measures reflect growing skepticism among some officials regarding the need for annual boosters for the general population. An estimated 100 million to 200 million Americans will remain eligible for vaccination under this updated framework, a significant reduction from the previous inclusion of nearly all individuals six months and older.
This change has drawn mixed reactions from health experts. Rick Bright, a former federal vaccine official, welcomed the clarity in these guidelines, stating, “Not everyone is at equal risk, and public policy should reflect that reality.” Conversely, critics argue that these new requirements bypass necessary input from independent experts, potentially limiting access to vaccines for those who wish to get vaccinated.
Concerns have also been raised about affordability, as limiting coverage could mean insurers may not pay for vaccines for all individuals. Dr. Michael Osterholm, director of the Center for Infectious Disease Research and Policy, emphasized that health decisions should ensure equitable access to vaccines for everyone.
Additionally, some experts warn of the ethical implications of requiring placebo-controlled trials for a vaccine that is already known to be effective. Dr. Offit, a vaccine expert at Children’s Hospital of Philadelphia, expressed concern that this could lead to lower availability and insurability of vaccines.
In summary, the FDA’s shift in policy may streamline the vaccination process for high-risk groups but leaves many unanswered questions regarding access and the future of COVID-19 vaccination in the United States.












