Health
ACA Premiums Set to Surge by 26% Ahead of Open Enrollment
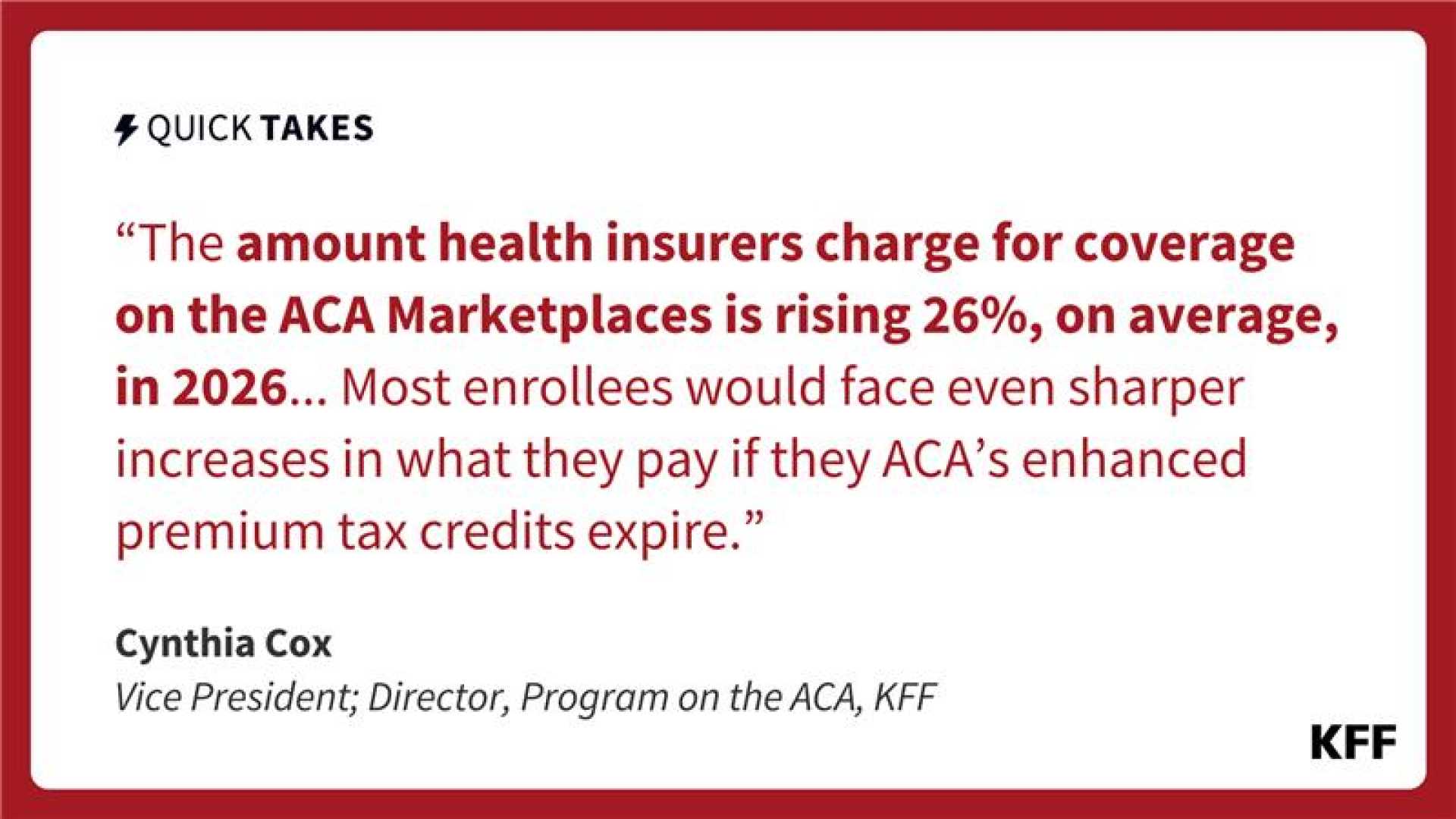
WASHINGTON, D.C. — Premiums for health coverage on the Affordable Care Act (ACA) marketplaces are projected to rise by an average of 26% in 2026. This announcement, made public on October 29, 2025, reveals a staggering 30% increase in states utilizing the federal Healthcare.gov platform, while states managing their own marketplaces face a 17% increase.
These premium hikes do not account for the anticipated expiration of premium tax credits, which could further escalate costs for enrollees. If the subsidies expire at the end of the year, those currently benefiting from them could see their monthly premiums more than double, increasing by an average of 114%.
The subsidy debate is intensifying in Congress, as Democrats push for an extension. In contrast, Republicans have said they will not support any measures until the government reopens following a shutdown that has lasted over a month.
According to an analysis by the Kaiser Family Foundation (KFF), various factors contribute to the looming premium increases, including escalating hospital expenses and the rising use of costly weight management medications. Additionally, healthy individuals may choose to forgo coverage if tax credits lapse, leading to further rate hikes.
Health insurers highlight the importance of maintaining health coverage, emphasizing that unexpected medical events can occur at any time. Experts suggest that reliance on insurance for only high-cost incidents should be favored to manage financial risks more efficiently. Ge Bai, a health policy professor at Johns Hopkins, noted, “Unless insurance returns to its core function… relying on it for most health care transactions will remain inefficient.”
The open enrollment period for 2026 starts on November 1 and ends in mid-December. Consumers who select plans before the subsidy situation is resolved can adjust their choices until the enrollment period closes.












