Health
Canada Considers One-Dose HPV Vaccination to Enhance Vaccine Efficiency
A recent modeling analysis suggests that Canada could improve efficiency and maintain cervical cancer prevention rates by switching from a two-dose to a one-dose human papillomavirus (HPV) vaccination program. According to the study published in CMAJ, one-dose, gender-neutral vaccinations could be significantly more efficient, even under pessimistic scenarios, if protection remains robust during peak sexual activity ages.
Dr. Chantal Sauvageau, an infectious diseases consultant and study author, highlighted the impact COVID-19 had on HPV vaccination rates, particularly among vulnerable groups. “The COVID-19 pandemic has impacted HPV vaccination in Canada, particularly among vulnerable population subgroups,” she stated. Dr. Sauvageau is affiliated with Quebec’s National Institute of Public Health and the University of Laval.
The study’s scenarios predicted that cervical cancer could be eliminated in Canada between 2032 and 2040 under a one-dose regimen. HPV contributes to other cancers such as oral, throat, and penile, which are mostly preventable via vaccination. Dr. Sauvageau added that a one-dose strategy would offer economic savings and programmatic flexibility, allowing for increased efforts in regions with low vaccination coverage to mitigate the pandemic’s effects on health programs.
Globally, nations are considering a shift to a single-dose HPV vaccine following the World Health Organization‘s recommendation in 2022. Canada’s National Advisory Committee on Immunization (NACI) began recommending a single-dose approach for ages 9-20 years this past July, aligning with countries like Australia and the United Kingdom. However, two doses remain recommended for older age groups and those with compromised immune systems.
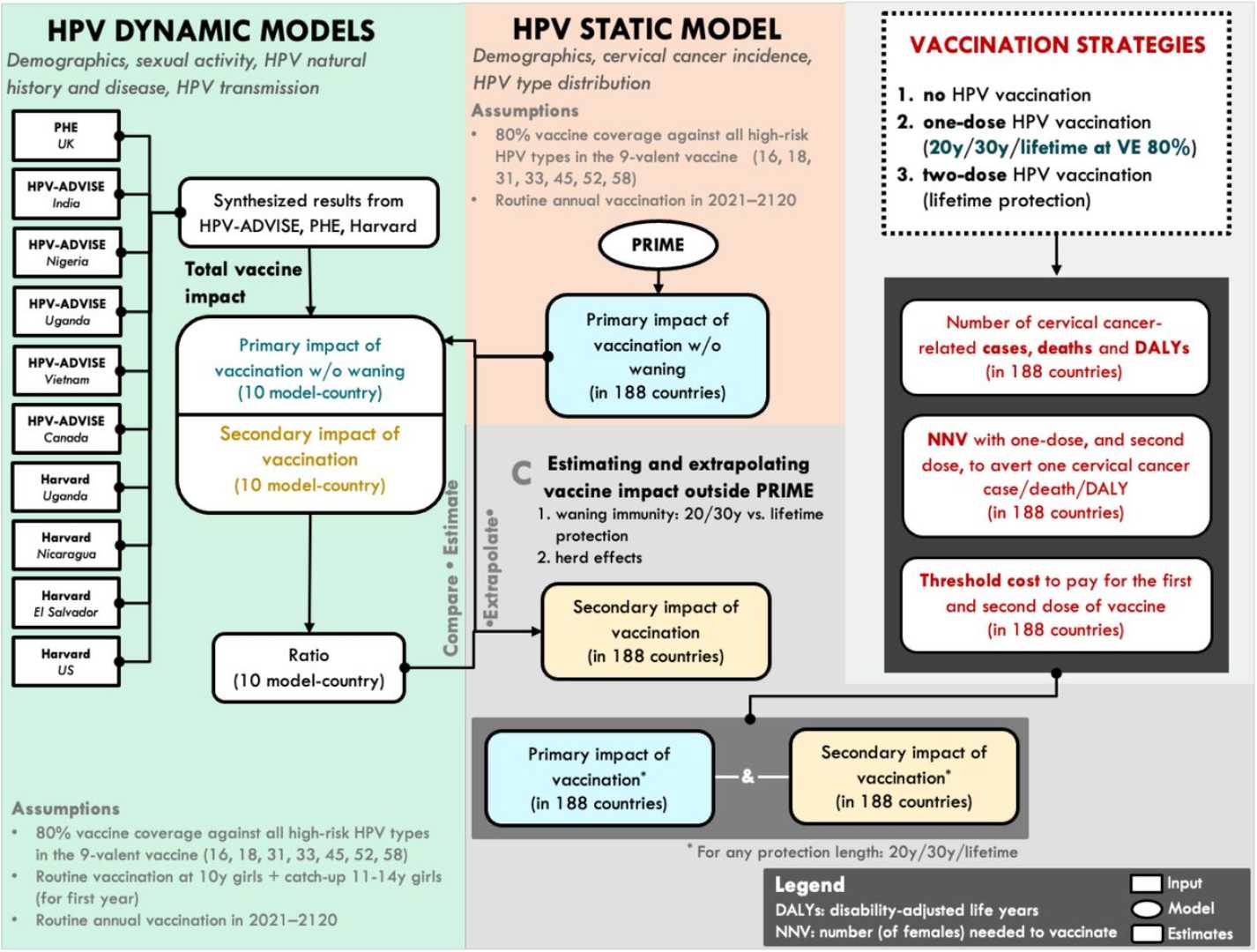
Using the HPV-ADVISE model, researchers analyzed vaccination programs in Quebec, with an HPV vaccine coverage of about 85%, and Ontario, with a lower coverage of about 65%. The study considered various one-dose scenarios with efficacy rates of 90% and 98%, predicting they would substantially reduce HPV-related infections and cervical cancer incidence compared to the current two-dose program.
While a one-dose program may lead to infections rebounding after 25-30 years due to waning efficacy, the model suggested that noninferior one-dose strategies could avert a similar number of cervical cancer cases as a two-dose approach. Notably, a one-dose program would require significantly fewer doses to prevent a single cervical cancer case, making it a more efficient use of resources.
Critics of the switch include the Federation of Medical Women of Canada, which issued recommendations to maintain multidose schedules due to their current proven effectiveness. Dr. Vivien Brown, chair of the group’s HPV Immunization Task Force, remarked, “Until more research on the efficacy of a single-dose schedule becomes available, healthcare providers and public health agencies should continue to offer patients a multidose schedule.”
The study involved funding support from the Public Health Agency of Canada, the Canadian Institutes of Health Research, and the Bill & Melinda Gates Foundation. Dr. Sauvageau and her colleagues declared no financial conflicts of interest.












