Health
CMS Drops Appeal, Forced to Recalculate Medicare Star Ratings for UnitedHealth
WASHINGTON, D.C. — The U.S. Centers for Medicare and Medicaid Services (CMS) announced Friday it will not appeal a court order requiring it to recalculate star ratings for UnitedHealth Group‘s Medicare Advantage plans, a decision that could significantly impact the insurer’s revenue.
The agency withdrew its notice of appeal just three days after filing it, without providing a reason for the reversal. The move comes after a Texas federal judge ruled in November that CMS acted arbitrarily in docking UnitedHealth’s star ratings based on a single unsuccessful test call. The case highlights ongoing disputes between CMS and insurers over the fairness of the star rating system, which helps consumers compare Medicare Advantage plans.
UnitedHealth, the largest Medicare Advantage provider in the U.S., argued in its lawsuit that CMS unfairly penalized some of its plans by reducing their ratings by half a star due to a failed test call seeking a foreign language interpreter. The insurer claimed the error was caused by the test caller, not its own systems, and that the rating adjustment could cost it millions in lost customers.
“CMS was arbitrary and capricious in docking the star ratings on the basis of a single call,” UnitedHealth stated in its lawsuit. The Texas judge agreed, ordering CMS to recalculate the ratings.
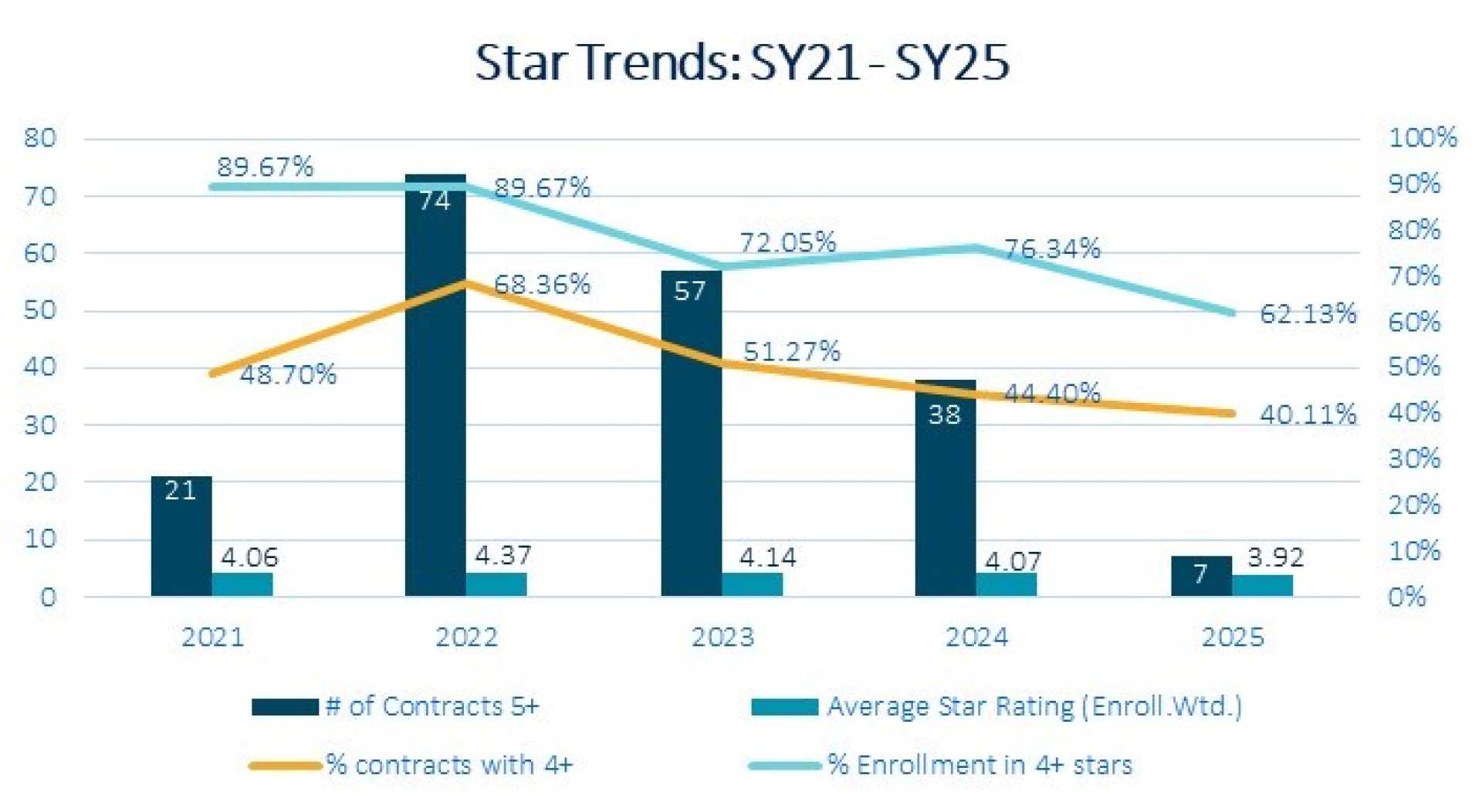
CMS assigns Medicare Advantage plans ratings of one to five stars based on quality and performance metrics. These ratings influence consumer choices and determine bonus payments to insurers. A half-star drop can significantly affect enrollment and revenue, as plans with four stars or higher receive additional funding from CMS.
Other insurers, including Elevance, Centene, and Humana, have also challenged CMS over alleged unfair star ratings. Earlier this year, CMS was forced to adjust ratings for Elevance and non-profit SCAN Health Plans after losing separate court rulings.
CMS declined to comment on the decision to drop the appeal, citing a policy restricting public statements by health agencies implemented during the Trump administration. UnitedHealth did not immediately respond to requests for comment.
Following the announcement, UnitedHealth Group shares rose 0.6% to $532.86. The company’s Medicare Advantage plans serve millions of Americans aged 65 and older, as well as some individuals with disabilities.
The case underscores the growing tension between insurers and CMS over the star rating system, which critics argue can be overly punitive for minor infractions. As Medicare Advantage enrollment continues to grow, the stakes for insurers and beneficiaries alike remain high.












